What is the best dosage of a vitamin to take for maximum benefits?
The FDA and NIH (Dietary Guidelines for Americans) develop vitamin guidelines using some of the physiological measurements available that show prevention of obvious disease symptoms. They recently have also started to give both an upper tolerance amount to stay below as well as the usual lower adequate amount. Most vitamin formulas stay within these guidelines. But there are a few that are over the upper recommended amounts and the upper limits can be exceeded by consuming a number of products each containing vitamins in the normal range. Plus the upper amounts may be exceeded not only by the supplement, but with the addition of vitamin fortified foods and certain food groups such as dairy. Harvard Medical on vitamins.
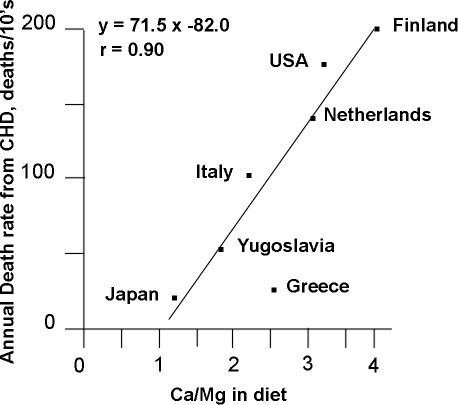
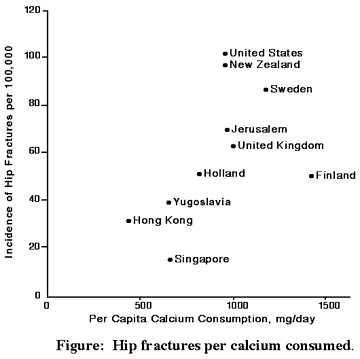
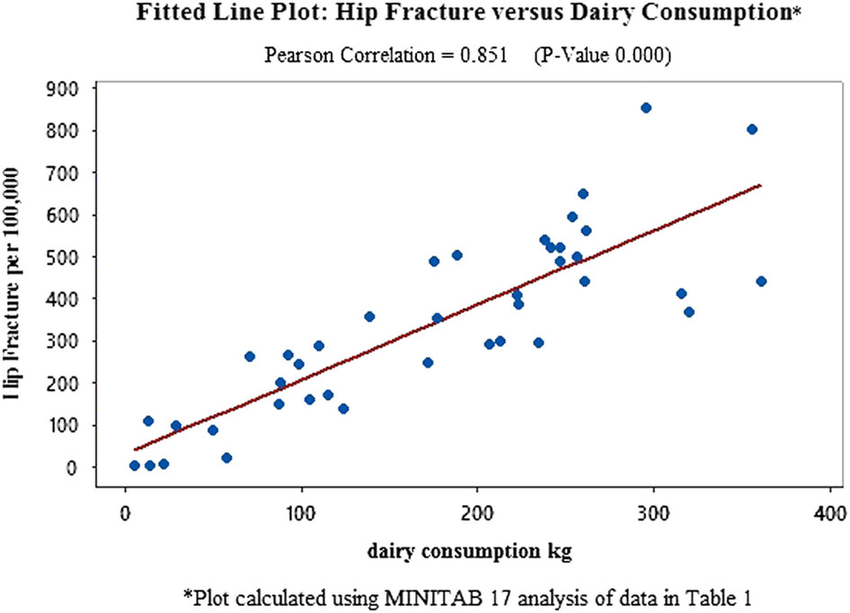
While absorption of vitamins in supplement form is important to know for proper dosages, it is also vital to explore what the body does with nutrients once inside the body, such as how they interact with each other or other elements and related processes. Calcium stimulates hormonal responses which are also influenced by essential fatty acids like the omegas 3 and 6.
SIDEBAR: The most appropriate dosages for nutrients in multi-vitamins might be 50% of the RDI, recommended daily intake. Dietary food supplies 50-80% of most nutrients.
A DOSAGE DISADVANTAGE
Over many years, vitamin supplement companies have used different methods to gain an apparent advantage over other vitamin Brands. One unfortunate way was to increase dosages giving the impression that "more is better" without actually having any scientific proof. The "B" vitamin complexes fall prey to this marketing ploy all too often. See below.
Most vitamins have a range or window of optimal benefits that is rather low, similar to the amounts nature supplies in foods. Absorption, assimilation, interference, reaction potential, plasma levels, and cellular levels need to be part of setting proper dosages. While the body has many adaptive methods to deal with nutrient loads outside the ideal window amounts, these methods often use up or interfere with other nutrients, energy, and vital processes. (Note: This next reference includes studies with high amounts of target nutrients, but is one of reasons nutrient levels in new vitamin criteria appear to be low, they are not, just the right amount for health.)
EXAMPLES OF TESTING METHODS
Measuring blood levels. Often Scientists measure the plasma or blood levels achieved from different dosages of vitamins. While this is important, it can be misleading for some nutrients like magnesium where Red Blood Cell levels also must be measured. Testing animals can yield different reading from human measurements as the two do not have identical uptake processes. Many studies use animals. Dosages affect absorption percentages. Some nutrients like vitamin B1 have greater absorption percentages at very small amounts and exhibit reduced percentages as dosages increase. Calcium also shows better absorption at lower amounts that at higher. This is often due to body protective mechanisms. It does not want to get to much of certain nutrients like iron into the body.
The BALANCED B VITAMIN MISTAKE
Forty years ago B Complex vitamins were mostly just low dosage liver or brewers yeast tablets. Next came the synthetics still in similar dosage patterns to the vitamin B amounts in liver and yeast. This formula pattern similar to foods had the eleven B complex vitamins in seemingly random amounts, but actually these amounts were somewhat balanced to body needs. Then, a vitamin company came out with what it called a "balanced" B complex. Almost all the eleven B vitamins were at the same amount, like most at 25 milligrams. This may have been "balanced" in that all had nearly the same amount, BUT it was not balanced according to the physiology needs and uses of B vitamins in the body. This represented a major step backwards from natural body wisdom and is unfortunately still the primary formula driver today. Only now the dosages are all 50 mg or even 100 mg. The 100 mg one is potentially damaging for a small minority of people. While a small amount of Vitamin B6 is needed for nerve health, at 100mg, the upper limit of NIH guidelines, a few cases have surfaced that exhibit beginning nerve damage. At dosages higher than 200mg of vitamin B6 adverse case percentages start to increase. ref
Check out the recommended amounts for B vitamins in the new Vitamin Criteria. Although they seem low, they are quite adequate for normal nutritional support. For vitamin B6 the amounts are 5-20 mg. Five mg is preferred, even 2.5mg is OK, with 20 the total for day. Also, it is a good idea to not take supplemental vitamins one or two days a week, like Sunday and Wednesday.the body simply does not need vitamins every day as it holds on to some for a while, especially fat soluble vitamins A, D, E, and K. Vitamin D for a couple of months. the water soluble B vitamins can take up to 11 days to completely clear out. vitamin B12 much longer. possibly up to a year.
Unique VITAMIN D
Vitamin D is unique in that it is not so much the dosage that matters, but rather the beginning blood level. There are many ways to arrive at the proper blood level range. Dosages range from 400 to 5000 IU. In 3 months, one reaches the peak increase from these doses of vitamin D. For every 100 units of D, your blood levels will increase about 1. Thus, if you are low at 15, taking 1500 IU for 3 months should get you to around 30, the proper level of the vitamin D storage level, as 25OHD, which has as its range between 20-40 ng/mL. With 30 the average.
Many say this is too low, but mortality associations pan out for these numbers. 30 ng/mL is the same as about 75 nmol/L. Just two different scales of measurement. Over 40 ng/mL, mortality again starts to slightly increase just like for low levels under 18. Make sure you understand which measurement unit your Doctor is taking about as this is vital information to get the right vitamin D dosage to put you into the proper range. Without measuring blood levels, the safe amount to take is about 2000 IU for no more than 3 months. After 3 months, back off to 600, or one 2000IU every 3-4 days. After 4 months, one may have to take D every day again to replenish levels, especially approaching winter since low sun exposure.
Differences in Forms of Vitamin D
The storage form of vitamin D is not the same as the hormone form which has 1000 times greater activity for cell binding attachment. Many Professionals equate the storage level with the hormone level, but this is not true. The storage form is more stable lasting 3 months where the hormone form only lasts 2-3 days. The storage form serves as the precursor material that the Kidneys make into the hormone form when it is needed. And while the two forms function separately, they are interconnected since the storage form has a 1000 times greater attraction to the vitamin D transport Binding Protein (DBP) in blood over the hormone form. This might be a method for the body to control the hormone D actions.
This control also reveals why it is important to not let the storage form get too high which might over-control or block out the actions of the hormone form in attaching to DBP for transport in blood. Especially since the storage form of D can also weakly bind to the vitamin D docks (called Vitamin D receptors, VDR) on cells where the hormone form does most of its work. After binding to cell docks, the hormone D form directs cells to build certain proteins for specific functions. One protein D produces is called LL-37. LL-37 has antibiotic actions to fight infections in the body. Another protein is called osteocalcin. It functions to attach calcium to bone crystals and also helps control blood sugar.
If the storage form of vitamin D is too low or too high, the actions of the hormone D form can be severely affected by a combination of these actions: control or interference with D binding protein (DBP) transport in blood, ability to form attachments with cell docking sites (VDR), plus the production of secondary D metabolites that control breakdown speed of hormone D. Cancer cells exhibit the ability to speed this breakdown and prevent new hormone D production. The secondary D metabolites are formed from the storage or hormone D forms. This is another method the body uses to control hormone D actions. Hormones are very powerful and a little goes a long way to make things happen in the body.
WRAP UP
The appropriate recourse is to get vitamin dosages within the correct window for amounts to maximize benefits with as little interference as possible. Remember too much vitamin E, mostly the isolate only alpha tocopherol form, interferences with vitamin K. There are many of these situations. The new vitamin criteria builds these factors into recommendations. Plus, it wisely recommends the proper use of all the vitamin family members for synergist functions.
Quite a few, if not most of certain vitamin studies referenced use the isolated or synthetic version of the isolated vitamin and this can influence results in an adverse manner. It is entirely possible that many of these studies would yield different results if the proper combinations of family vitamins were studied. In many cases, the different family forms either compliment and protect each other, often by maintaining a balance of opposite effects under unique conditions. Such as when the normally antioxidant beta carotene** turns to into an pro-oxidant in smokers and increases lung cancer rate. ref Vitamins can react with metals to increase oxidation stress. ref This was only a test tube study and most likely other factors in the body control these potential functions at normal food nutrient amounts. But, it again shows that more is not better for many if not most vitamins.
There is a optimal window or range of vitamin amounts that needs to be respected for maximum health benefits. That is just how the amazing body functions.
**Beta carotene in over 95% of multiple vitamins contain only one form, the all-trans beta carotene form, and miss out on the synergistic functions of the other form of beta carotene found in nature, 9-cis. It is the 9-cis form after converting into 9-cis retinoic acid (vitamin A form) in the body that combines with vitamin D stimulated VDR on cell walls to fulfill the vitamin D functions of not only protecting bones, but also to fine tune the immune system against, among other conditions, cancerous cells.
Where is the logic for using a non participating, or very low action form of beta carotene for an influence beyond the scope of that form? Is this the state of vitamin science and the scientific method today?
Remember the Doctor Researcher that compared the body levels for the different family forms of vitamin E in heart patients versus healthy individuals. The form of vitamin E used in most research studies, d'alpha tocopherol, was the same in each group. It was d'gamma tocopherol that was lower in heart patients than in controls. Generally, a vitamin that is found lower in people with a disease condition would be considered an associated factor, and studies would increase that vitamin to test the theory. ref Is the wrong form of vitamin E being tested, or is there a synergism among vitamin E family member amounts that needs to be respected?
Since observation studies show higher vitamin E diet has a protective effect on heart health, the family effect appears to be corrective since food contains many vitamin E family members. ref <Alpha tocotrienol is one of the family members of vitamin E. For more, see article.
 Thursday, August 30, 2018 at 12:29AM
Thursday, August 30, 2018 at 12:29AM