Is there an ideal vitamin D blood level?
CAUTION: The following information needs to have this precaution added. One of the functions of active, short-lived, hormone form of vitamin D is to increase absorption of calcium from food in the intestinal tract. But, it turns out this process may not just pinpoint calcium, it also increases a few other minerals, also including toxic metals like lead. ref Studies show that children exhibiting higher vitamin D levels sometimes also have higher blood levels of lead. This could either be due to increased lead absorption or from lead released out of bones, another side effect function of vitamin D. To prevent the absorption of toxic metals, the essential minerals like magnesium, phosphorus, zinc, and copper must be at adequate amounts. Since a number of populations have wide degrees of deficiency for some of these minerals, it is prudent to avoid known toxic metal containing foods such as sprouted grass grains, certain vegetables, plus rice protein powders. Children are more susceptible to lead uptake than adults. This is one reason it may be prudent to monitor vitamin D dosages until science settles this issue. ref ref< vitamin C too.
Vitamin D supplements are available in 2 forms, vitamin D2 and D3. While some research says both are equal, over the long haul, they are not equal with D3 showing higher blood levels than from D2. ref
Here is a review that studied research to arrive at the "Ideal" blood vitamin D level for 25-OHD3. The blood level this review decided upon as ideal was between 35-40 ng/mL, or 90-100 nmol/L. This information was put together almost 9 years ago. There have been some modifiers since then as noted below. One exception might include males with a family history of prostate cancer. In this case, the safe vitamin D level might be 20-25. At higher levels, the enzyme needed to activate the hormone form of vitamin D is down regulated.
From the last article on VDBP, standing for Vitamin D Binding Protein, the ratio of VDBP to 25-OHD3 must now be a factor that could modify this amount either way. Then there is the fact that while most cancers exhibit less risk at increasing D levels, there are some like pancreatic and prostate that show more risk as vitamin D levels increase above natural, or at least as these higher levels may influence calcium behavior.
Of Interest: There is also the possibility this goes deeper into the relationship of calcium to magnesium that is really involved. If magnesium levels are adequate, which they are not in 64% of population, ref, then vitamin D actions and calcium levels have less impact and it is the magnesium level that is critical factor. ref ref ref
Here are the health factors from the above review that played a role in this determination: "...maintain muscle strength, prevent falls, improve dental health, and prevent cancer (especially colorectal cancer). Weaker evidence for vitamin D includes preventing multiple sclerosis, other cancers, arthritis, hypertension, and tuberculosis, as well as solving insulin problems (diabetes mellitus)."
Here are the ways 2 items from this list are aided by vitamin D. Vitamin D induces the production of LL-37, an infection fighter. This natural antibody shows action for the health of the mouth and gums and also lungs. ref
Diabetes, multiple sclerosis, and rheumatoid arthritis are all types of autoimmune diseases. ref
Optimal Blood Levels May Vary
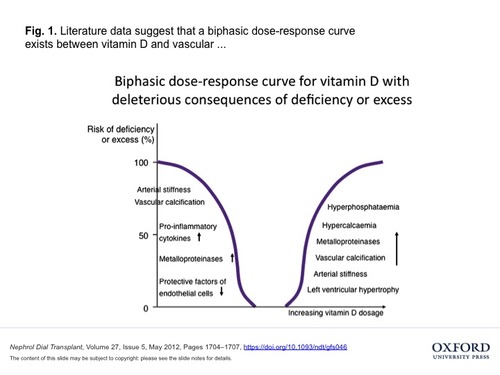
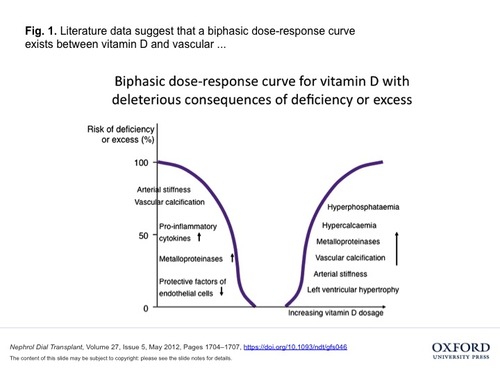
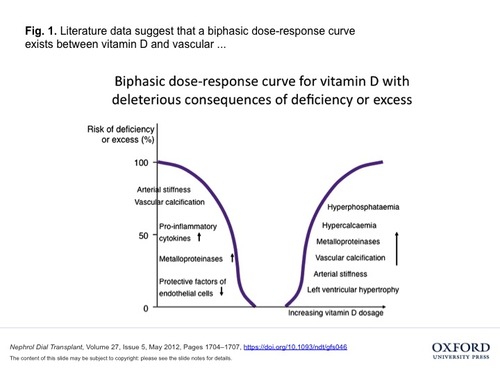
It is entirely possible that there could be an optimal vitamin D level that is slightly different for each health condition or that varies by individuals as well due to genetics. Here is a report showing that the level of vitamin D exhibiting the lowest CRP blood level is 21ng/ml. This Johns Hopkins study shows that at both lower and higher vitamin D levels the amount of CRP goes up. CRP stands for C-Reactive Protein, an indicator of inflammation in the body that is linked with cardiovascular disease. ref But, not all people with elevated CRP will develop cardiovascular disease.
The Ideal Optimal Vitamin D level has to factor in all these differences. These differences may be reported as if they represent the optimal D level. For some cancers, the optimal D level might be over 50 ng/ml while at this level, other adverse conditions might surface in other diseases or issues, like for prostate or pancreatic cancers. Since the ideal vitamin D blood level may vary, an could vary, an optimal range for the ideal vitamin D level would be necessary.
SIDEBAR: New research shows that a certain level of the storage form of vitamin D is needed to participate in ideal bone remodeling between bone building cells and bone tearing down cells. That amount from animal studies is 32 ng/mL. Some tests of Americans puts vitamin D levels low at 15 ng/mL. To get that up to 32 ng/mL, a supplement dosage of 1700IUs would be needed for 3 months. But if at 25 ng/mL, only 700 IU would be needed for a few months.
Wrap Up
Copied here is a wise summation from the review referenced at the beginning of this article. "Why not surpass the number of 35-40 ng/ml as some experts have suggested? Unfortunately, higher does not mean better. Medical research is replete with examples of where a little higher helped, but more was not necessarily better. Supraphysiologic levels beyond what is now recommended in this manuscript is not yet supported in medical literature. It is interesting that some studies (for example, in the area of prostate cancer) have not yet found considerable benefits to achieving such higher vitamin D levels (Mucci & Spiegelman, 2008). In fact, it has been suggested that long-term significant increases in vitamin D could be detrimental. Thus, some experts suggest that there is no harm of carrying high vitamin D levels (70 ng/ml or more for example), but this recommendation is based on acute and not chronic observations."
Acute means short term while chronic involves over a longer length of time. Just because vitamin D3 is available with 5,000 -10,000 units does not mean it is safe for everyone. ref One Brand of vitamin D3 with 5,000 IUs says to take 1 or 2 daily, while another says to take one every other day. The latter one would average 2500 per day, a much safer "higher" amount to take for the general public.
Taking 5,000 per day would over 3 months increase the ng/ml number by anywhere from 30-50. The lower number in people who weigh more and the higher for people who weigh less since fat absorbs vitamin D. If one was at 15 ng/ml to start, a typical average in USA, that would mean a new total of 45-60, possibly slightly increasing adverse risk for some people. Taking 2500 would increase starting number by 15-25, arriving at a total between 30-40. ref After 3 months, no further increases occur unless the dosage gets larger. If more than 2500 is taken, it might be wise to do so with medical supervision knowing the starting number.
The issue here is not that 5,000 to 10,000 of vitamin D is toxic. It is that these amounts could increase the blood calcium level too high with resulting detrimental consequences, or it could interfere with the hormone form of vitamin D when it is needed to stimulate vitamin D receptors. This issue is still in question, as is what the next reference found.
VITAL CAUTION: (This is for CKD, chronic Kidney disease, who might have conversion problems and may not be the same for normal healthy individuals) Here is a reference that reveals it is better to slowly build up vitamin D levels if they are low. A rapid increase of blood vitamin D levels may have undesirerable consequences. It increases the mechanism to speed the destruction of vitamin D into a non active form and eliminate it our of the body. This rapid D increase accomplishes this destructive action by activating certain enzymes. Plus, the rapid increase also has little effect to lower PTH levels to protect calcium in bones. (The higher doses were from IV) What if any effects oral higher dosages of vitamin D over 2500 IU might have for this occurrence is still unknown. Research with higher dosages is not looking at this aspect. Slowly increasing vitamin D blood levels with conservative D amounts does not activate these enzymes but does significantly lower PTH levels. ref ref
Bottom Line: It appears that lower PTH levels are more important than higher vitamin D levels to safe against bone loss in the elderly. ref
Not all research agrees with what the last reference found. But, if this is proven to be valid, better to opt now to follow since no harm. Quite a bit of research looks at the relationship between PTH and vitamin D blood levels. BUT, it is the hormone form of vitamin D (1,25(OH)2D3) that interacts with PTH and not so much the measured storage form of D (25OHD3) in blood. Also, (24,25(OH)2D3 is rarely measured which is the form of D that controls and destroys the hormone D form.
MEN, PROSTATE, & VITAMIN D
Here is one report revealing that men with higher vitamin D levels as well as higher DBP levels increase their risk for prostate cancer. Also mentioned in this report is that pancreatic cancers are higher in people with high vitamin D and low DBP levels.
SIDEBAR: Vitamin D Binding Protein (VDBP) levels influence the effects of vitamin D. A higher VDBP to vitamin D molar ratio appears to reduce the benefits of vitamin D. More of the vitamin D is VDBP bound so less is available as "free" vitamin D, the bio-active form. How this molar ratio can be impacted is still under research. DBP has a few different forms that further modify how DBP influences vitamin D actions. There are 3 major DBP forms that significantly impact vitamin D.
Copied here is the conclusion from a VDBP study on Diabetes: "Conclusions: Low 25(OH)D levels were associated with risk for diabetes among whites, but not blacks, with the strongest associations observed among those genetically predisposed to high DBP levels. The effects of vitamin D supplementation for the prevention of diabetes may differ by race and bio available vitamin D levels." ref
Note: 25-OHD3 has a 1000 times greater affinity for D Binding Protein than the hormone form of D, 1,25(OH)2D3. While the Hormone form has a 1000 times greater attraction to vitamin D receptor sites on cells. Can you see a possibility that too high a pool of vitamin D as 25-OHD3 might interfere with the action of the hormone form at cellular receptor sites? They are a synergistic team and function together. ref
SIDBAR - Another Vital Function for Vitamin D
Copied here to prevent it getting lost, a study showing that Vitamin D slows down the speed of telomere shortening prolonging the life of leukocyte cells. This should reduce the development of some age-related diseases.
"Am J Clin Nutr. 2007 Nov;86(5):1420-5.
Higher serum vitamin D concentrations are associated with longer leukocyte telomere length in women.(not in Men)
Richards JB, Valdes AM, Gardner JP, Paximadas D, Kimura M, Nessa A, Lu X, Surdulescu GL, Swaminathan R, Spector TD, Aviv A.
Twin Research and Genetic Epidemiology, St Thomas' Hospital, King's College, London School of Medicine, London, United Kingdom. brent.richards@kcl.ac.uk
Abstract
BACKGROUND: Vitamin D is a potent inhibitor of the proinflammatory response and thereby diminishes turnover of leukocytes. Leukocyte telomere length (LTL) is a predictor of aging-related disease and decreases with each cell cycle and increased inflammation.
OBJECTIVE: The objective of the study was to examine whether vitamin D concentrations would attenuate the rate of telomere attrition in leukocytes, such that higher vitamin D concentrations would be associated with longer LTL.
DESIGN: Serum vitamin D concentrations were measured in 2160 women aged 18-79 y (mean age: 49.4) from a large population-based cohort of twins. LTL was measured by using the Southern blot method.
RESULTS: Age was negatively correlated with LTL (r = -0.40, P < 0.0001). Serum vitamin D concentrations were positively associated with LTL (r = 0.07, P = 0.0010), and this relation persisted after adjustment for age (r = 0.09, P < 0.0001) and other covariates (age, season of vitamin D measurement, menopausal status, use of hormone replacement therapy, and physical activity; P for trend across tertiles = 0.003). The difference in LTL between the highest and lowest tertiles of vitamin D was 107 base pairs (P = 0.0009), which is equivalent to 5.0 y of telomeric aging. This difference was further accentuated by increased concentrations of C-reactive protein, which is a measure of systemic inflammation.
CONCLUSION: Our findings suggest that higher vitamin D concentrations, which are easily modifiable through nutritional supplementation, are associated with longer LTL, which underscores the potentially beneficial effects of this hormone on aging and age-related diseases."
This study did not measure people taking extra Vitamin D, it just found that people with higher levels of vitamin D from sun and food had longer telomere length, which is a good thing, compared to people with the lowest blood levels of vitamin D. (The 3 levels used for vitamin D measured in at 16 ng/mL, 29 ng/mL, and 50ng/mL)
REMEMBER: Cancer and maybe other diseases have the ability to lower the conversion of vitamin D and also speed the elimination out of the body of the hormone form of vitamin D. Thus, a low vitamin D reading needs a complete body examination to eliminate the possibility of a non-observable cancer. Most studies fail to show benefits from improved vitamin D levels AFTER a disease is present.
Bottom Line: It appears that lower PTH levels are more important than higher vitamin D levels to safeguard against bone loss in the elderly. ref ref
 Saturday, December 11, 2010 at 4:28PM
Saturday, December 11, 2010 at 4:28PM