Why Hearts Attack
 Monday, March 19, 2012 at 1:03PM
Monday, March 19, 2012 at 1:03PM The pendulum is swinging back, Cholesterol is taking a backseat to chronic Inflammation as the driver of heart disease and cancer. It is difficult to pin it only on cholesterol when half of heart attack events occur in individuals with cholesterol levels considered safe (within acceptable levels). article ref ref ref (C-Reactive Protein indicates inflammation somewhere in body)
NEW UPDATE BELOW

Here is everything and more you would ever want to know about cholesterol, a vital ingredient for health. And the chart that says it all. Next is info the Medical Profession uses to support more statin use. ref Someone has to justify this with these facts. ref And NOW, 2015, the US Government makes startling admission on dietary cholesterol. ref
Insight: Here are the results of a large analysis of dietary patterns on CVD from 42 Countries. Interesting results. Saturated fat is taking a back seat.
The body uses EPA, an omega 3 fat, as the controller of the inflammatory process through messengers it produces and sends out to stop the enzyme processing of both Omega 3 and Omega 6 pathway cascades, especially of Omega 6 into Arachadonic Acid (AA). AA produces messengers that participate in pro-inflammatory actions. A healthy ratio is needed between these factors which a balanced diet (before 20th century) maintained. It is now known that there is a very profound balance needed between Omega 3 EPA and DHA and omega 6 AA that not only influences fatty acid balance and messenger production, but also on transcription factors that help regulate inflammatory gene expression. Most notably NF-kB. This one you will hear more about as new cancer theories put it front and center in cancer promotion and growth. ref
This important research from almost 28,000 Women's Health Study shows chronic inflammation connected to fatty acid profile balance between omega 6 and omega 3 is vital to controlling and preventing chronic inflammatory caused heart and stroke conditions.
"BACKGROUND (study referenced above copied here in case link is lost)
Both C-reactive protein and low-density lipoprotein (LDL) cholesterol levels are elevated in persons at risk for cardiovascular events. However, population-based data directly comparing these two biologic markers are not available.
METHODS
C-reactive protein and LDL cholesterol were measured at base line in 27,939 apparently healthy American women, who were then followed for a mean of eight years for the occurrence of myocardial infarction, ischemic stroke, coronary revascularization, or death from cardiovascular causes. We assessed the value of these two measurements in predicting the risk of cardiovascular events in the study population.
RESULTS
Although C-reactive protein and LDL cholesterol were minimally correlated (r=0.08), base-line levels of each had a strong linear relation with the incidence of cardiovascular events. After adjustment for age, smoking status, the presence or absence of diabetes mellitus, categorical levels of blood pressure, and use or nonuse of hormone-replacement therapy, the relative risks of first cardiovascular events according to increasing quintiles of C-reactive protein, as compared with the women in the lowest quintile, were 1.4, 1.6, 2.0, and 2.3 (P<0.001), whereas the corresponding relative risks in increasing quintiles of LDL cholesterol, as compared with the lowest, were 0.9, 1.1, 1.3, and 1.5 (P<0.001). Similar effects were observed in separate analyses of each component of the composite end point and among users and nonusers of hormone-replacement therapy. Overall, 77 percent of all events occurred among women with LDL cholesterol levels below 160 mg per deciliter (4.14 mmol per liter), and 46 percent occurred among those with LDL cholesterol levels below 130 mg per deciliter (3.36 mmol per liter). By contrast, because C-reactive protein and LDL cholesterol measurements tended to identify different high-risk groups, screening for both biologic markers provided better prognostic information than screening for either alone. Independent effects were also observed for C-reactive protein in analyses adjusted for all components of the Framingham risk score.
CONCLUSIONS
These data suggest that the C-reactive protein level is a stronger predictor of cardiovascular events than just the LDL cholesterol level and that it adds prognostic information to that conveyed by the Framingham risk score." --end of copy
UPDATE: A new enzyme has been associated with inflammation in arteries. Adding measurements of this enzyme to CRP levels in chest pain patients gives even greater alert to the likelihood of a pending heart attack. The enzyme myeloperoxidase, or MPO, is made in white blood cells. This enzyme is produced and at higher concentrations when arteries are inflamed and have rupture-prone fatty deposits. ref
Remember, inflammation and resulting C-Reative Protein are present in all cases of artery diease, BUT not all people with high C-Reative Protein and inflammation have artery diesease. MPO represents one additional key to explaining why this is so.
A new drug, Lovaza, made of a highly refined fish oil is showing promise in protecting against heart attacks. The omega 3 fats in fish oil protect the cell membranes covering plaque and prevent rupture through an interactive process acting between platelets in the blood and intestinal wall cell membrane integrity. Lowering triglyceride levels might be one mechanism responsible for these omega 3 actions. ref Plus, omega 3 fish oils also increase the LDL particle sizes. Larger is better.
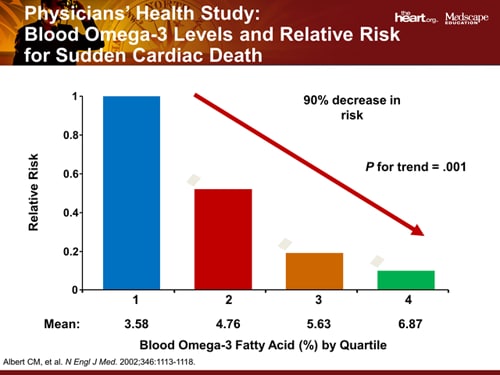 This again brings back into play the dietary ratio of omega 6 to omega 3 fatty acids, or at least the level of omega 3 at sufficient amounts to offer protection against and modulate the pro-inflammatory cascade effect. Trans-fats are especially damaging here and the falling heart attack rate from the 1970s onward might in large part be influenced by the health food industry offering healthier alternatives and generating awareness. This change in heart attack rate direction started about 10 years BEFORE statins were introduced. The downward decline did not change or vary after Statin introduction. The Scientific talk of late has been about the anti-inflammation effects of Statins rather than about cholesterol lowering. The facts now overwhelmingly support this.
This again brings back into play the dietary ratio of omega 6 to omega 3 fatty acids, or at least the level of omega 3 at sufficient amounts to offer protection against and modulate the pro-inflammatory cascade effect. Trans-fats are especially damaging here and the falling heart attack rate from the 1970s onward might in large part be influenced by the health food industry offering healthier alternatives and generating awareness. This change in heart attack rate direction started about 10 years BEFORE statins were introduced. The downward decline did not change or vary after Statin introduction. The Scientific talk of late has been about the anti-inflammation effects of Statins rather than about cholesterol lowering. The facts now overwhelmingly support this.
Very Interesting! A complete index to references for the many inflammatory markers in the body. Notice CRP, Fibrinogen, and Hyaluronate. Here is a research study showing statins also have an effect on fibrin formation that helps CVD outcome. Copied from this study, "the inhibitory effect of statins on the mevalonate pathway is involved in the regulation of some key steps of coagulation and fibrinolysis processes."
This next very techno reference reveals Statins interfere with the PAL-1 pathway that is involved in inflammation and wound healing.(1) ref This is very new research and will need many years of duplication and testing before any public exposure erupts. The vital piece of info here is that PAL-1 triggers PXR and PXR triggers PAL-1, and PXR is involved with Drug resistance and cancer spreading. This is one of the pathways cancer cells might hyjack and use to protect against chemotherapeutic drugs and speed the proliferation of new cancer cells. (2) ref
Copied from ref (1): Plasminogen activator inhibitor type 1 (PAI-1) is a multifunctional protein that has important roles in inflammation and wound healing. Its aberrant regulation may contribute to many disease processes such as heart disease. The PAI-1 promoter is responsive to multiple inputs including cytokines, growth factors, steroids and oxidative stress. The statin drugs, atorvastatin, mevastatin and rosuvastatin, increased basal and stimulated expression of the PAI-1 promoter 3-fold. Copied from ref (2): PXR is expressed in several cancer tissues and the accumulating evidence strongly points to the differential role of PXR in cancer growth and progression as well as in chemotherapy outcome. In cancer cells, besides regulating the gene expression of enzymes and proteins involved in drug metabolism and transport, PXR also regulates other genes involved in proliferation, metastasis, apoptosis, anti-apoptosis, inflammation, and oxidative stress. In this review, we focus on the differential role of PXR in a variety of cancers, including prostate, breast, ovarian, endometrial, and colon.
Interesting History of heart disease here (<moved page, searching for another) Heart disease was almost unknown before the 1900's.
Please read the abstract for the above study. It reveals a possible eplanation for sudden heart attacks when other observable evidence is not found. Phosphate tocivity. Here are the foods that are high in phosphates: article
- Dairy foods.
- Beans.
- Lentils.
- Nuts.
- Bran cereals.
- Oatmeal.
- Colas and other drinks with phosphate additives.
- Some bottled ice tea.
Since many of these foods have other valubale nutrients, moderation is the key. Plus, grains and legumes also contain phytes which bind with phosphorus to limit absorption. This is another reason Vegetables are used since they do not contain phosphates. Balance between calcium, phosphorus, and magnesium gain significance with this concept. ref Kidneys play a large role in this balance. Also of consideration are the functions of vitamin D and K to direct and control the placement of these minerals in the proper body structures and not in soft tissues or artery walls.
It appears that both low and high phosphate blood levels are associated with higher risk for caridac events. ref
This represents another situation where Health Agencies are failing to protect Public Health. While food processors are adding phosphates to many propared foods, even those not considered high in phosphates, science is finding upset balance in minerals as the cause of or associated with numerous diseases.